Problems with cell’s skeleton and energy production: how a single gene defect can affect both neuronal development and immune system function
Researchers in Finland and Norway have discovered a gene defect that causes a novel inherited immune deficiency. The same gene, DIAPH1, has been previously shown to cause SCBMS syndrome, a rare genetic disease associated with severe brain development defects.
The results help to gain a deeper understanding of the biology of SCBMS and will provide a basis for the exploration of new therapeutic approaches.
A novel immunodeficiency syndrome caused by pathogenic variants in the DIAPH1 gene has been identified by an international collaborative study led by Professors Janna Saarela and Johanna Uusimaa. DIAPH1 has been previously associated with a rare inherited neurodevelopmental disorder characterized by early-onset epileptic seizures, severely delayed psychomotor development, cortical blindness, and microcephaly, also referred to as SCBMS.
New findings published in this study show that patients with disease-causing variants leading to a lack of the DIAPH1 protein product have deficient T and B cell functions in addition to the neurological phenotype. They are also prone to developing hematological malignancies. These new findings will help with reaching a genetic diagnosis for patients presenting with neurodevelopmental disorder or syndromic immune deficiency.
“The characteristic neurological symptoms and signs present soon after birth and lead clinicians to suspect a group of neurodevelopmental disorders - including SCBMS - that can be verified by genetic testing. However, the combined immune deficiency, particularly if unnoticed, can be life-threatening to the patients”, says Dr. Saarela, Director of the Centre for Molecular Medicine Norway (NCMM).
The new findings expand the SCBMS phenotype and highlight the need to monitor for immune system defects in children suffering from this disease.
This study also provided novel neuroradiological and neuropathological data on SCBMS. Brain MRIs of the patients demonstrated several structural alterations, and neuropathological examination of the brain occipital cortex showed abnormal neuronal lamination, gliosis and total neuronal loss.
This study also provided novel neuroradiological and neuropathological data on SCBMS. Brain MRIs of the patients demonstrated thin chiasm and optic nerves, as wells as white matter and cortical abnormalities in bilateral occipital lobes. Furthermore, neuropathological examination in autopsy and immunohistochemical stainings of the brain occipital cortex showed abnormal neuronal lamination, gliosis and total neuronal loss.
The researchers showed how deficiency of DIAPH1 impairs the activation and proliferation of T lymphocytes and maturation of B lymphocytes, predisposing the patients to viral and bacterial infections and malignancies. CRISPR-Cas9 based gene removal of DIAPH1 in T cells of the healthy donors replicated the activation defect and proved the link between DIAPH1 and poor T cell function.
The study included both Finnish and Omani patients. All the currently known Finnish patients have been identified and clinically examined by the specialists at the Oulu University Hospital. As seen in other rare diseases in Finland, a single Finnish founder mutation has been enriched in the Finnish population and all described patients carry the same homozygous loss-of-function variant. The Omani patients investigated in this study have a different DIAPH1 variant, which also leads to loss of the protein and to immune deficiency in addition to SCBMS, a phenotype combination first described in this study.
DIAPH1 regulates reorganization of the cytoskeleton in activated T lymphocytes
The scientists found that patients’ T cells exhibited impaired adhesion capacity, altered spatial organization of the microtubule cytoskeleton and had a more circular structure.
“Our results provide evidence for the role of DIAPH1 in the regulation of cytoskeletal organization. This is an interesting finding, since also several other cytoskeletal defects are known causes for immunodeficiency”, explains Meri Kaustio, the first author of the study.
“In this study we also discovered a novel role for DIAPH1 in regulating the mitochondrial oxidative phosphorylation (OXPHOS) system, which explains clinical signs characteristic to patients with mitochondrial diseases”, says Johanna Uusimaa, Professor of Paediatric Neurology at the University of Oulu, a co-senior author of the study.
Reetta Hinttala, Associate Professor at the University of Oulu continues, “Surprisingly, both the lack and over expression of the DIAPH1 protein caused isolated deficiency of mitochondrial respiratory chain complex IV, as we saw in patient cells and cell models.”
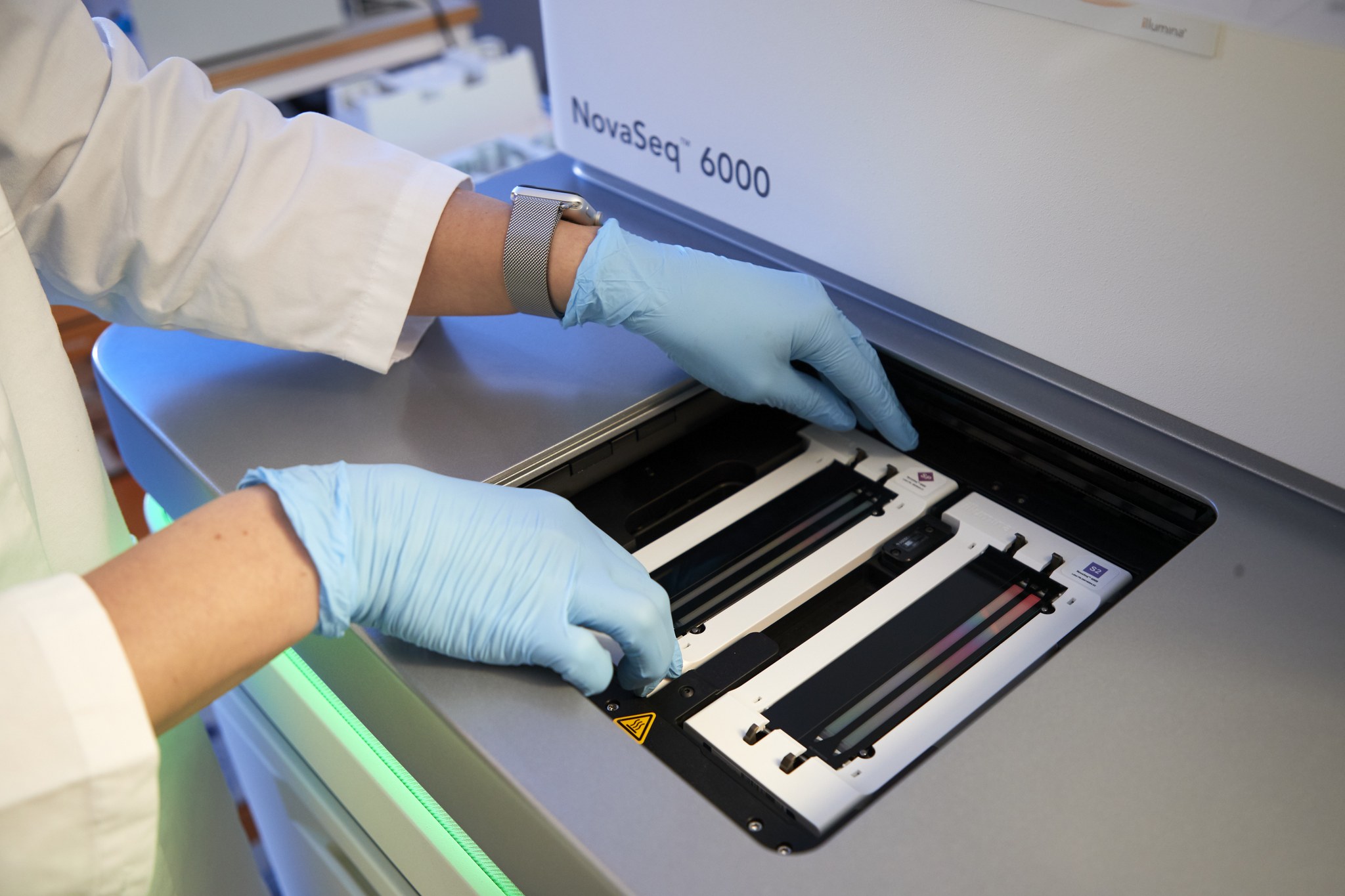
Exome sequencing technique gives a better insight into genetic diseases and how they operate
Whole-exome sequencing enables both the discovery of previously unknown disease genes and the identification of atypical clinical manifestations of known monogenic syndromes, thus broadening our understanding of their underlying characteristics.
“The close interaction between clinical diagnostic sequencing and the PID research program has enabled us to identify several novel PID genes. It has also provided a molecular diagnosis for patients suffering from yet undescribed rare immune deficiencies,” comments Janna Saarela.
Prof. Saarela is the Director of the Centre for Molecular Medicine Norway (NCMM). Her research group is shared between NCMM and the Institute of Molecular Medicine Finland (FIMM), where she was previously assistant director and head of the FIMM Technology Centre. FIMM and NCMM share many similarities in terms of research expertise and interests. The Saarela group’s research focuses on understanding the biological pathways and pathogenic mechanisms behind rare and common immune diseases.
Collaborative research on rare diseases
This scientific work was possible thanks to an international collaboration of the two Nordic EMBL Partnership for Molecular Medicine institutes, the Institute for Molecular Medicine Finland (FIMM) at the University of Helsinki and the Centre for Molecular Medicine Norway (NCMM) at the University of Oslo, together with researchers and clinical doctors from the University of Oulu, Oulu University Hospital, University of Eastern Finland, Kuopio University Hospital in Finland, the Royal Hospital and Sultan Qaboos University Hospital in Oman and the Rockefeller University in US.
Special thanks go to prof. Marjo Renko (Kuopio University Hospital), prof. Terhi Tapiainen (Oulu University Hospital), prof. Timo Hautala (Oulu University Hospital) and Dr. Tariq Al Farsi (the Royal Hospital, Oman).
The results of the work were recently published in the Journal of Allergy and Clinical Immunology: Loss of DIAPH1 causes SCBMS, combined immunodeficiency and mitochondrial dysfunction. Kaustio et al., 2021DOI:https://doi.org/10.1016/j.jaci.2020.12.656