Bandung Revisited: from Rural Hygiene to Primary Health Care
Niels Brimnes (Associate Professor - Aarhus University)
Forty years ago, from 6 to 12 September 1978, representatives from 134 countries and 67 organizations and agencies met in Alma-Ata (today Almaty) in what was then the Soviet Republic of Kazakhstan to promote the concept of ‘Primary Health Care’. The conference was organized by the World Health Organization (WHO) and UNICEF and resulted in the ‘Declaration of Alma-Ata’, which urged “all governments, all health development workers and the world community to protect and promote the health of all the people of the world” through the adoption of Primary Health Care.[1]
The strategy of Primary Health Care had been high on the WHO agenda for some years. A 1975 World Health Assembly resolution requested the Director-General to promote the development of Primary Health Care activities and to organise a major conference to that effect.[2] The large meeting in Alma-Ata in September 1978 was the result of this and arguably the culmination of the Primary Health Care movement.
While the ideas and strategies embedded in the concept of Primary Health Care appeared to be new, there was in fact a solid connection to a conference held 41 years earlier under the auspices of the League of Nations Health Organization (LNHO): the 1937 conference on rural hygiene in Bandung, Indonesia. Emphasizing and discussing the most important of these connections, this blog argues that ideas promoted under the auspices of the League of Nations had an important and enduring legacy in the post-war decades.

The Alma-Ata conference was held in the Lenin Convention Centre
The Declaration of Alma-Ata and the principles behind Primary Health Care
The declaration of Alma-Ata referred explicitly to the notion of a ‘New International Economic Order’ (NIEO), as adopted in a resolution by the UN General Assembly in 1974, and thus openly sided with the demand for a global redistribution of wealth promoted by many developing countries in the political climate of the early 1970s. An official pre-conference report called for “the transfer of a greater share of health resources to the underserved majority of the population”, and requested affluent countries to commit themselves “to a more equitable distribution of international health resources”.[3] An internal document used more dramatic language. Primary Health Care was here presented as “a code word describing a health related response to the international and national cry for social equality and justice with equal emphasis upon the developing world and the underserved groups of many countries”.[4]
The particular approach to health care sanctioned at Alma-Ata challenged policies providing sophisticated medical technology to “the privileged few” and suggested an alternative that sought to make essential health care universally accessible.[5] This alternative was embedded in three principles: intersectoriality, community participation and appropriate technology.
For want of a better word, I use ‘intersectoriality’ as a reference to the insistence that health issues be seen in the context of general social and economic development. As stated in the post-conference report “Primary Health Care is an integral part of the socioeconomic development process”.[6]
Community participation was defined in the pre-conference report as “the process by which individuals and families assume responsibility for their own health and welfare” and as a principle that enabled them “to become agents of their own development instead of passive beneficiaries of development aid”. In the language of later decades, community participation was ‘empowerment’.[7]
Appropriate technology meant that apart from being scientifically sound, the technology applied through the health services should be simple, affordable and “in keeping with the local culture.” It did, therefore, challenge a pharmaceutical industry, which preferred to develop expensive, sophisticated drugs to elites across the world.[8]

‘Barefoot doctors’ undertaking farm work in China. Along with other types of semi-skilled community health workers, the barefoot doctors were a source of inspiration for primary health care. Photo from 1970.
The notion of appropriate health technology was closely interwoven with an emphasis on community health workers, who had not received extensive or clinical training. References were made not only to the importance of nurses, ‘feldshers’ and the famous Chinese ‘barefoot doctors’, but also to the value of ‘indigenous’ practitioners of other medical traditions and women.[9]
Remembering Bandung 1937
If Primary Health Care appeared to be new, it was because it stood in contrast to the dominant approach to international health in the preceding decades, embodied more than anything else in the Malaria Eradication Programme (MEP). Launched by WHO in 1955, the dream of eradicating malaria had to be abandoned in 1969, when it was adjusted into a less ambitious ‘control’ programme. Many saw this as WHO’s greatest failure and the decade from the abandonment of MEP to the Alma-Ata declaration can easily be interpreted as a period in which WHO sought to reformulate the basis of its policy and to regain the prestige lost.[10]
The contrast between Primary Health Care and MEP is striking. MEP was narrowly confined to the health sector. It was a centrally devised campaign, designed and carried out by public health bureaucrats in Geneva, New York and other metropolitan centres. The technologies applied – mainly DDT spraying – was anything but appropriate and acceptable to local communities. Rather than using people and resources from within the community, it was conducted by outside ‘spraying teams’ insensitive to local needs.[11]
The visions and principles enshrined in Alma-Ata did not, however, emerge as a simple reaction to the flaws of MEP. Primary Health Care was the 1970s avatar of a tradition to think of health in broad, social terms, which went back to the first half of the century. In the 1930s it was known as ‘social medicine’ or ‘rural hygiene’ and this approach arguably culminated at a conference held under the auspices of the LNHO in Bandung, Indonesia in 1937.
One of the main architects behind Primary Health Care, WHO Director-General Halfdan Mahler, was well aware of the roots of the ‘new’ approach. Socrates Litsios, who worked in the WHO section developing the concept of PHC, ‘discovered’ the report from the Bandung conference and found striking similarities. Litsios drafted an article, which was published in Mahler’s name a few months before the Alma-Ata conference, and which explicitly discussed the legacy of the 1937 conference and the obvious links to the conference he was preparing.
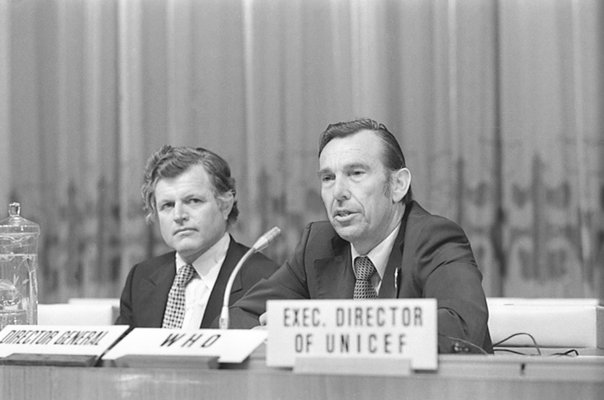
WHO Director-General Halfdan Mahler at the Alma-Ata conference with US senator Robert Kennedy.
The article recognized that the delegates at Bandung had understood how health was connected to broader economic, social and educational developments, had realised the importance of community participation and had been sceptical about schemes superimposed by governments.[12] It then reviewed the principles of Primary Health Care, in the form Mahler had presented them to the World Health Assembly in 1975, and noted: “The similarity between these principles and the conclusions reached in 1937 cannot be denied. Clearly, PHC is not “new”.” The article then rhetorically asked the obvious question: “Why has it been necessary to resurrect ideas that were put forward decades ago? What happened between 1937 and 1975?” [13]
The answer was that the delegates in Bandung had made one crucial mistake: recommending that every country should strive to attain the “highest scientific level of theoretical and practical training”. This inevitably led to a preference for advanced medical technology and a health service biased towards catering for the few and wealthy.[14] Primary Health Care was now being developed as an alternative “that has more than once been recognized as the best road to take”, and while it in many ways reiterated the principles stated in Bandung, it differed by finding more space for various kinds of community health workers including “traditional healers and local midwives”. [15]
The League of Nations Conference on Rural Hygiene
The Bandung conference on rural hygiene is a debated and often celebrated moment in the history of international health. Theodore Brown and Elisabeth Fee described it as a ‘milestone event’ in health and development and emphasized the similarities with Alma-Ata.[16] According to Iris Borowy, the conference in Bandung:
“might have been one of the first, if indeed not the first major international event in public health in which Asian voices were heard and representatives of non-Western regions were allowed to speak for themselves and challenge the idea of one universal Western model for world health.”
Borowy further found the Conference to be “both the high point and the end” of the LNHO’s work in Asia.[17] More modestly, Sunil Amrith described Bandung as perhaps the first “formal dialogue on questions of health and welfare which was at once imperial, and international”.[18] Randall Packard saw it as the ‘culmination’ of the interest in rural reconstruction and hygiene outside Europe, but noted in a more critical vein, that it also reflected the continued entanglement of international health organizations and colonial medicine.[19]
There are significant similarities between Bandung and Alma-Ata, but it is worth having a closer look at the former, in order to determine more precisely, to what extent the notion of Primary Health Care discussed at Alma-Ata was a continuation of – or a return to – the ideas on rural hygiene discussed in Bandung.
First – as noted by Packard above – Bandung was an event situated firmly within a colonial world order, and the majority of the participants were colonies under European authority. While Bandung did not call for changes in the colonial, international order, Alma-Ata emerged as a cry from a decolonized world for a more just distribution of resources invested in health. Bandung did call for redistribution of resources within nations and colonial possessions, though only in scattered references to a need for ‘land reform’.[20] In Packard’s analysis, the discussions in Bandung did highlight the social and economic problems behind poor health, yet “at almost every turn, the conference participants backed away from recommendations that would have radically changed the status quo in order to improve rural hygiene in their countries”.[21] Interestingly, Alma-Ata was as cautious to demand internal reforms. Presumably, this was in adherence to the principle of “non-interference in the internal affairs of other states”, as stated in the NIEO declaration.[22] If colonialism was not up for discussion in Bandung, the privileges of national elites in the global south was not a target in Alma-Ata.
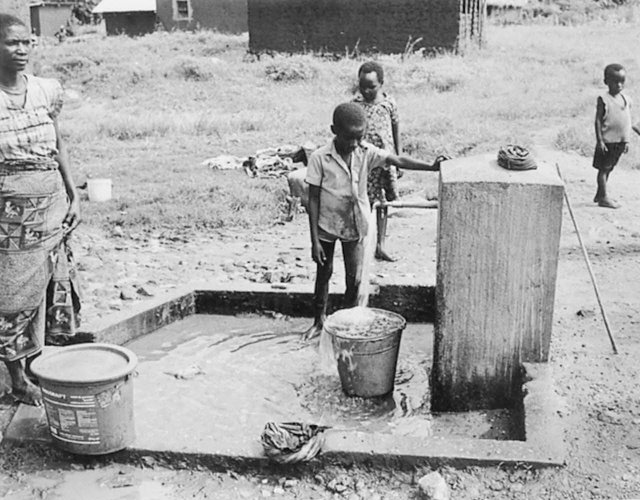
An adequate supply of safe drinking water was emphasized as crucial to rural hygiene at the Bandung Conference and became one of the essential elements of primary health care. Photo from 1980.
‘Intersectoriality’ was openly embraced in Bandung. In the introductory part of the report, it was emphasised that efforts to improve public health would fail unless they coincided with improvements carried out in fields such as agriculture and economy, and the conference gladly noted that the delegations consisted of representatives from several sectors apart from health:
“This may be taken as a positive indication that those responsible for the medical services and health protection of the rural populations in the East realise that their work is made difficult, if not impossible, unless activities in the fields of economics, sociology, agriculture and education are carried on at the same time.”[23]
This concern had a clear parallel in the preparation for Alma-Ata, where invitations were deliberately sent to both the ministries of health and the ministries of foreign affairs in order to reach stakeholders beyond a narrowly defined circle of health officers.[24]
Likewise, community participation formed a significant part of the discussions in Bandung, and ‘Rural Reconstruction and the Collaboration of the Population’ was one of the five overarching themes on the conference agenda. The discussions on this theme noted that it was necessary “to work through the people, and avoid, as far as possible, imposing systems from above” and produced resolutions that advocated village committees.[25] Another panel impressed that “the people should be led, not driven”. This phrase indicates, however, that even if the active collaboration of communities was solicited, it was in a more patronising way, than forty years later in Alma-Ata. Village communities had to be supervised or ‘led’ by a ‘committee of management’ consisting of government experts and several speakers emphasised that “improperly trained personnel cannot secure the confidence of the rural people …".[26]

Malaria control without DDT. Health worker engaged in a ‘count’ of the larvae-carrying mosquitoes in Afghanistan. Photo from 1971.
The emphasis on appropriate technology is another obvious similarity between Bandung and Alma-Ata. One example is the ‘naturalistic’ method of controlling malaria, which was endorsed by the delegates in Bandung in a way that could have been copied directly into the reports from Alma-Ata. Naturalistic methods of controlling malaria were seen as “relatively inexpensive” and they could “suitably be carried out by the peasants themselves”.[27]
When it comes to the corollary of appropriate technology, the promotion of semi-skilled auxiliary personnel or community health workers, the similarities between Bandung and Alma-Ata are less obvious. This was the issue identified by the ‘Mahler’ article as the crucial mistake of Bandung. It can be argued, however, that Bandung’s position on the role of semi-skilled health workers was more complicated than argued.
Borowy has shown how the authors in charge of compiling the important preparatory report for Bandung not only held views strongly in favour of semi-skilled personnel, but also saw indigenous medical traditions as a resource.[28] In the introductory section to the report from the conference, this issue was first framed in an open and inconclusive way. It was noted that there existed two answers: to insist on academic training up to the standard found in central universities or to accept that diplomas were issued to less educated health workers – both emphasised as equally important.[29] The resolutions adopted by the conference insisted, as noted by Mahler, that “every country should, in the sphere of medical education, attain the highest level of theoretical and practical training …”, but they also referred to the importance of “adequately training a large body of auxiliary personnel”.[30]
The ‘Mahler’ article seems, therefore, to have over-interpreted Bandung’s insistence on highly qualified doctors. Statements on the auxiliary personnel from Bandung came, in fact, quite close to match the positive qualities, which Alma-Ata conferred on the ‘community health worker’, the ‘barefoot doctor’ and the indigenous practitioner.

Traditional medicine: Preparation of herbal medicaments in China. Photo from 1977.
The legacy of the League
It is not surprising, that Mahler and WHO sought to identify an important difference between the health strategy advocated in Bandung before World War II and the new concept of Primary Health Care he was promoting in the lead up to the Alma-Ata conference. They obviously needed to brand PHC as genuinely new and as a strategy that had ‘learned’ from mistakes in the past. It is equally unsurprising that it is possible to demonstrate profound similarities between Bandung and Alma-Ata, also where Mahler and WHO claimed differences. Ideas branded as ‘new’ are rarely without solid connections to the past, and when it comes to international cooperation in the late 20thcentury, the League of Nations is an obvious place to look. The case of the Primary Health Care strategy and its fundamental principles of intersectoriality, community participation and appropriate technology is no exception.
References:
[1] ‘Declaration of Alma-Ata’, in Primary Health Care (PHC). Report of the International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978, Geneva: WHO, 2-6.
[2] WHA 28.88 in Handbook of Resolutions and Decisions of the World Health Assembly and the Executive Board, II, 1973-84, Geneva: WHO 1985, 64-65. The third Ten Years of the World Health Organization, 1968-1977. Geneva: WHO 2008, 293.
[3] Primary Health Care (PHC). A joint report by the Director-General of the World Health Organization and the Executive director of the United Nation’s Children’s Fund, Geneva & New York: WHO and UNICEF, 1978, 12-13, 16.
[4] The Third Ten Years, p. 302.
[5] PHC. A joint report, 7-8
[6] PHC. Report of the International Conference, p. 17.
[7] PHC. A joint report, 20-21
[8] PHC. Report of the International Conference, p. 19.
[9] PHC. A joint report, 31-34.
[10] Randall Packard A History of Global Health. Interventions into the Lives of Others,Baltimore: Johns Hopkins University Press (JHUP), 2016, 231.
[11] Randall Packard The Making of a Tropical Disease. A Short History of Malaria, Baltimore: JHUP, 2007, 150-76, particularly 168-69.
[12] Halfdan Mahler ‘Promotion of Primary Health Care in Member countries of WHO’, Public Health Reports, 93 (2), 1978, 107. For Litsios’ involvement in the drafting of the article, see Litsios, Socrates, ‘The Long and difficult road to Alma Ata: A personal reflection, International Journal of Health Services, 32 (4), 2002, 720.
[13] Mahler, ‘Promotion’, 108.
[14] Mahler, ‘Promotion’,108. Mahler quotes the Bandung Conference report.
[15] Mahler, ‘Promotion’, 109, 111.
[16] Theodore M. Brown and Elizabeth Fee, ‘The Bandoeng Conference of 1937: A Milestone in Health and Development’, American Journal of Public Health, 98 (1), 2008, 42-43.
[17] Iris Borowy, Coming to Terms with World Health. The League of Nations Health Organisation 1921-46. Frankfurt a.M.: Peter Lang 2009, 355-56.
[18] Sunil S. Amrith, Decolonizing International Health. India and Southeast Asia 1930-65. Basingstoke: Palgrave 2016, 38.
[19] Packard, A History of Global Health, 84.
[20] ‘Report of the Intergovernmental Conference of Far-Eastern Countries on Rural Hygiene’, Geneva: League of Nations 1937, 26, 56.
[21] Packard, A History of Global Health, 85.
[22] ‘Declaration on the Establishment of a New International Economic Order’, para 4 a., A/RES/S-6/3201, http://www.un-documents.net/s6r3201.htm, accessed 8. September 2018.
[23] ‘Report of the Intergovernmental Conference’, 23, see also 9.
[24] The Third Ten Years, 299.
[25] ‘Report of the Intergovernmental Conference’, 51, 54-55.
[26] ‘Report of the Intergovernmental Conference’, 38, 54, 41. See also Packard, History of Global Health, 86.
[27] ‘Report of the Intergovernmental Conference’, 92.
[28] Borowy, Coming to Terms, 351.
[29] ‘Report of the Intergovernmental Conference’, 8, 35.
[30] ‘Report of the Intergovernmental Conference’, 44.
Images:
1) Courtesy of WHO:[ref. WHO_A_012613]
2) Courtesy of WHO: [ref. WHO_A_014450]
3) Courtesy of WHO: [ref. WHO_A_000695]
4) Courtesy of WHO/Harry Anenden [ref. WHO_A_015715]
5) Courtesy of WHO/Paul Amasy [ref. WHO_A_000747]
6) Courtesy of WHO/Robert H. Banneman [ref. WHO_A_014465]
